Brachial plexus root derivation (C5-T1). Broad appreciation of the root / trunk / division / cord structure.
Detailed knowledge of which nerves derive through which cord NOT required.
Appreciation of the potential for plexus damage based upon its position in the axilla
Curriculum
Axilla is a well protected region on 3 sides – Superiorly, Laterally and Medially, and it hosts the important neurovascular bundle of Upper limb. It’s like a bridge between the neck and upper limb. The contents are prone to injury in trauma if Axilla is involved or if the arm gets pulled too much.
The Axillary artery gives some branches in the Axilla but the most notable ones are the “Anterior and Posterior Circumflex humeral arteries”.
The Anterior circumflex supplies the Head of Humerus and Shoulder joint.
The Posterior circumflex also supplies the Shoulder joint. It travels along the surgical neck of Humerus and anastomoses with Anterior circumflex laterally.
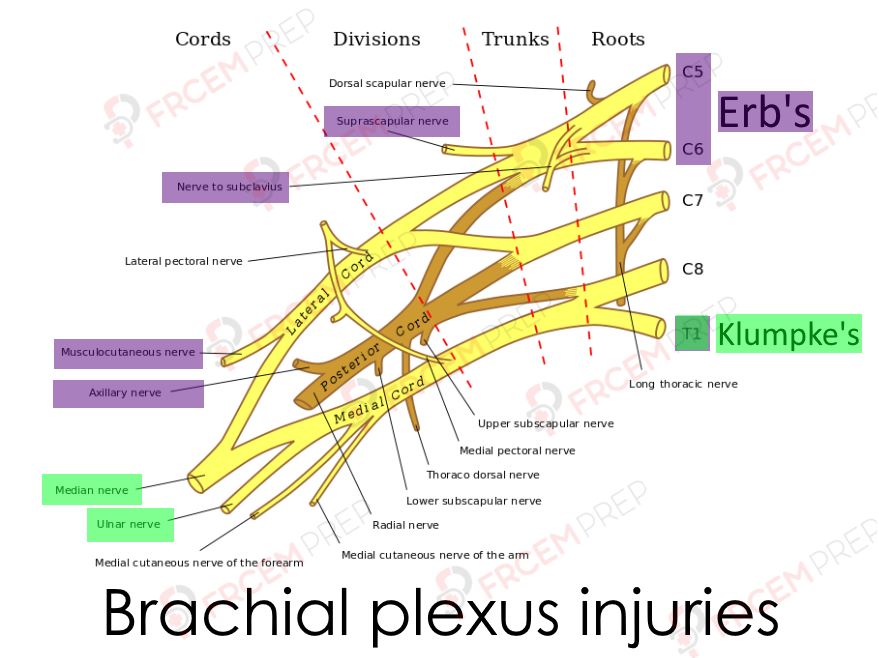
Image Modified from Brachial_plexus.jpg:Mattopaedia at en.wikipediaderivative work: Captain-n00dle (talk), MissMJ, Public domain, via Wikimedia Commons
Image shows the origin of Brachial plexus from C5 to T1 spinal roots. Roots merge to form Trunks and Trunks divide (divisions). Divisions merge to become cords. Do not get into detailed knowledge of nerve origins for this exams.
Applied anatomy of brachial plexus injuries should be known.
Erb’s palsy
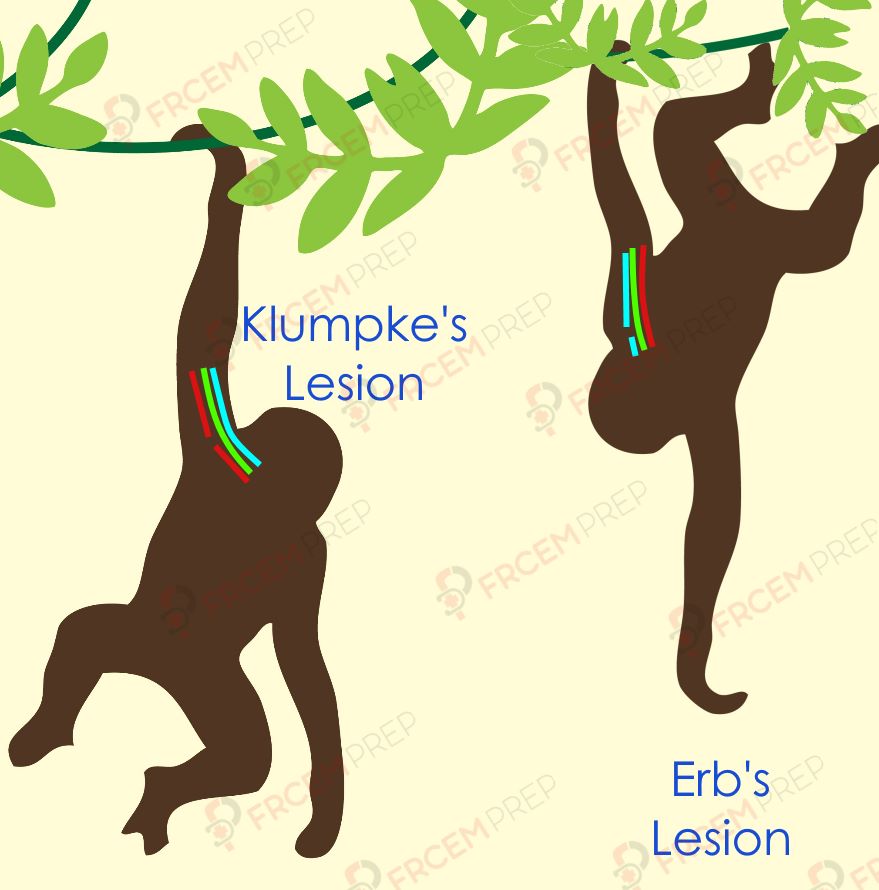
Excessive increase in the angle between the neck and shoulder will cause a stretch (or even tears) of the nerve roots of C5 and C6. (like in cases of difficult birth with breech delivery if the head is stuck and arm is pulled excessively or in cases of shoulder trauma).
Nerves with C5 or C6 roots: musculocutaneous, axillary, suprascapular and nerve to subclavius will be affected.
Muscles Paralyzed: The above affected nerves will lead to paralysis or weakness of
Shoulder stabilizers – Supraspinatus, infraspinatus, Teres minor, subclavius and Deltoid
Upper arm flexor (anterior) compartment – Biceps brachii, Brachialis, Coracobrachialis,
Movements affected – it’ll be easy if you know the functions of the above muscles.
@ shoulder – Abduction, lateral rotation of arm, and flexion
@ Forearm – supination of forearm
Sensory deficits: Loss of sensation down lateral aspect of arm, (axillary and musculocutaneous nerves).
Limb posture: Limb is medially rotated by the unopposed action of pectoralis major. The forearm is pronated due to the loss of biceps brachii function. The wrist extensor weakness leads to weakly flexed posture.
The waiter’s tip posture, characteristic of Erb’s palsy.
Klumke’s palsy
Excessive abduction of arm as in holding on to a tree branch when falling down and the entire body weight causing traction on lower roots of Brachial plexus.
Nerves affected : T1 root derived nerves are affected – ulnar and median nerves.
Muscles affected : The flexor muscles in forearm are also supplied by the ulnar and median nerves, but served by different roots and are not affected. But the lumbrical muscles are affected. They normally flex the metacarpophalangeal (MCP) joints and extend the interphalangeal (IP) joints, so their paralysis will cause the opposite effects.
Limb posture : Intrinsic hand muscles are paralyzed due to Ulnar nerve involvement, leading to “claw hand” [From unopposed Extension of the MCP and flexion of the IP joints].
Sensory loss – Loss of sensation along medial side of arm.